Cornea Transplants
For St. Petersburg & Clearwater, FL
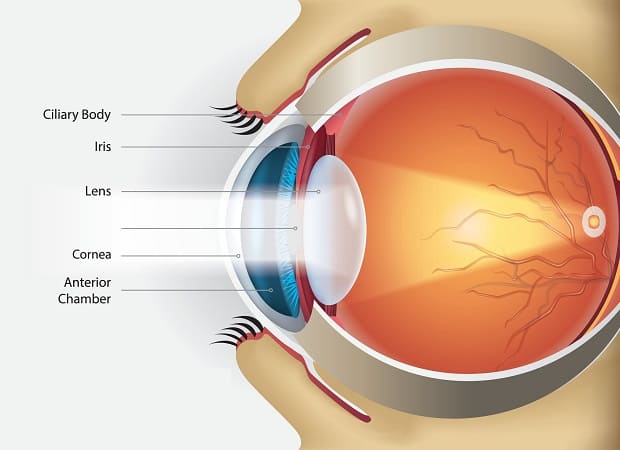
Your vision relies on a healthy, round cornea located at the front of your eye. When this vulnerable surface is damaged, swollen or scarred from trauma or disease, it can’t focus light, causing glare and blurry vision. A cornea transplant removes the damaged cornea and replaces it with cornea tissue from a human donor that is clear and healthy.
St. Michael’s Eye & Laser Institute is home to world-class Ophthalmologists who believe in continuing their education and using the most advanced technologies and techniques to restore your vision and ocular health. We are a three-generation, family-owned eye care and surgical center and the only North Florida center honored as an Alcon Center of Excellence. You can trust that your ocular health is in excellent hands during your eye exam at our Largo office, where we will discuss your cornea transplant options.
Types Of Cornea Transplants
The cornea is the clear surface of your eye that is made of three main layers: the epithelium (surface layer), stroma (middle layer) and endothelium (innermost layer). The middle and bottom cornea layers are separated by “Descemet’s membrane,” which is a dense matrix that is nearly transparent.
There are several types of cornea transplants. Some operations remove the entire cornea, while others focus on specific layers of the cornea. The type of cornea transplant used for your procedure is based on the condition of your current tissues.
Full Thickness Cornea Transplant
Full thickness cornea transplants replace the surface and inner layers of the cornea. Penetrating keratoplasty (PK) is the traditional option for cornea implants. In this procedure, the central cornea that is damaged or diseased is surgically removed and replaced with a donor cornea that is a similar size. The donor tissues are secured with sutures by our experienced surgeons. PK is a safe procedure with predictable results and typically restores full vision.
Recovery from full thickness transplants is longer than with other options, and there is a higher risk that your body’s immune system will reject the new cornea tissue. Donated corneas are tested to ensure they’re healthy and safe to use for transplantation.
Partial Thickness Cornea Transplant
Some eye conditions damage the inner layers of the cornea and leave the outer layers in good condition. Endothelial keratoplasty replaces the damaged cornea layer with healthy donor tissue and is called a partial cornea transplant as it leaves the outer layer intact. Where a full thickness transplant removes and replaces all three layers of the cornea, these options focus on specific layers to improve rejection rates, shorten recovery and restore optimal eye health:
- Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK): The DSAEK procedure removes the innermost cornea layer and replaces it with donor tissue. The benefits include few (if any) stitches, the lowest rejection risk, and most of the cornea is left intact. DSAEK is a good option for Fuch’s Dystrophy, which only damages the endothelial (bottom) layer.
- Deep Anterior Lamellar Keratoplasty (DALK): DALK is the opposite of DSAEK in some ways. The procedure leaves the endothelial layer and replaces the outer layers with donor corneal tissue. DALK provides results on par or better than the results of PRK and greatly reduces the risk of tissue rejection. It is used for certain keratoconus cases and offers a shorter recovery than other cornea transplants. Laser-assisted DALK can provide greater precision at the graft site and in shaping the donor tissue for optimal fit and a stronger graft.
Descemet’s Membrane Endothelial Keratoplasty (DMEK) is another partial thickness cornea transplant that replaces a single layer of the cornea (endothelial) for exact replacement with donor tissue.

Cornea Transplant Recovery
You can expect some discomfort and stinging or a feeling like something is stuck in your eye after a cornea transplant. These issues are often managed with over-the-counter pain medications. Our eye surgeon will cover the treated eye with a plastic shield to wear until your follow-up visit the next day. Prescription eye drops are used to prevent infection and reduce the risk of tissue rejection. The postoperative eye drop schedule is critical for cornea transplant success. Follow your post-op instructions to the letter and contact our office with any questions or if you start to feel severe pain.
Our Ophthalmologists recommend taking a few days off work or several weeks if you work in a dusty environment or lift heavy objects regularly at your workplace. Your vision will improve over time and may take a full year to stabilize as the grafted tissue heals.

What Is Keratoconus?
Keratoconus is a corneal condition that causes the transparent dome at the front of the eye to bulge and thin, morphing into a cone shape. The misshapen, weakened cornea causes light sensitivity, glare, blurry vision, frequent prescription changes and sudden or worsening cloudy eyesight. Keratoconus may affect both eyes and is typically worse in one eye.
People often develop this condition between 10 and 25 years old, and the thinning and bulging can progress for 10 years or longer. While glasses, various contact lenses and corneal collagen cross-linking can manage the early stages of keratoconus, aggressive treatment with a cornea transplant may be needed to halt disease progression in advanced cases.
Cornea Transplant Cost
Any transplant surgery is going to be costly. Tissue transplantation requires experienced medical professionals and involves many moving parts, such as a surgical team, hospital and donor bank. St. Michael’s Eye & Laser Institute is among the top 1% of cornea transplant centers worldwide, and our patients know they’re in excellent hands for their surgery.
It’s estimated that an outpatient cornea transplant can cost $13,000 for an outpatient procedure without insurance, and this price estimate goes up to $28,000 for inpatient surgery. This cost also depends on the type and extent of cornea transplant, such as a partial thickness procedure (DSAEK, DMEK or DALK cornea transplants). While your insurance provider may cover a portion of your cornea transplant costs, we understand the financial burden of restoring eye health and offer financing options, including CareCredit, to help you reach better vision with affordable payments. You may need prior authorization or approval for a cornea transplant with your insurance provider.
Cornea Transplant Recovery And Results
The best ways to ensure your eye heals after a cornea transplant are to follow our eye doctors’ directions to the “T” and attend every follow-up visit. Make sure you take your prescription eye drops and oral medications precisely when you are supposed to and wear your protective eye shield or eyeglasses as directed to protect the transplanted tissue while you heal. You may have to take certain medications for several months to help your body accept the transplanted tissue.
Don’t put pressure on the eye, and avoid touching or rubbing anywhere near the eye. Depending on the form of cornea transplant, you may need to lie down for a while after surgery to help the new tissue stay in place. That includes sleeping on your back and staying in this position as much as possible for up to several days or longer.
You may have significant differences in vision in the transplanted eye versus the other, which can be mitigated with eyeglasses or contacts while you recover. Your eyesight can change quickly after a transplant, and regular appointments at our Largo office are essential during recovery.
Our eye doctors can’t predict how your body will react to the cornea transplant. It’s a complex procedure that comes with some risks, such as infection, increased eye pressure, bleeding, retinal problems and rejection of the donor cornea. Complete recovery may take up to a year, but patients with successful cornea transplants enjoy good, healthy eyesight for years.
Learn More About Cornea Transplants
Our skilled Ophthalmologists are available to answer your questions. Contact St. Michael’s Eye & Laser Institute to schedule your comprehensive eye exam and learn more about cornea transplants.
 Patient Portal
Patient Portal  Online Payment
Online Payment  Doctor Referral
Doctor Referral  Financing
Financing